 www.MountPleasantMagazine.com
www.MountPleasantMagazine.com
|
www.ILoveMountPleasant.com|
www.BestOfMountPleasant.com58
high risk of developing into breast cancer. It’s uncommon
and is primarily found in women between 40 and 50.
Invasive ductal carcinoma is a more urgent matter since
it is cancer that has begun to spread. Kathleen opted for a
double mastectomy to assure the best possible long-term
outcome. It was followed by three months of chemotherapy
– every three weeks at MUSC in Mount Pleasant – which
was not as bad as she expected. She experienced weight loss,
fatigue and loss of appetite, but, fortunately, no nausea.
“The worst part was losing my hair,” Kathleen said.
A positive person by nature, she was able to maintain
a good attitude. It also clarified that time is finite and not
to be wasted. She and her sister, who recently underwent
treatment for ovarian cancer, made good on their promise
to travel “sometime.” This past May, they went to Hawaii
on a “sisters’ survivors” trip.
“It makes you feel your mortality,” Kathleen said. “Take
nothing for granted.”
Her four children were “very supportive,” especially
during the stressful weeks between the mammogram and
the final diagnostic results.
“I truly felt lucky,” she said. “I said OK, what is the
silver lining? It was caught early and I got new boobs!”
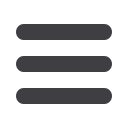
The emoTional Side
Cindy Eley
had a brush
with breast
cancer in 2007
when a mam-
mogram showed
a few calcifica-
tions, but the
real trouble
showed up years
later, on July
14, 2011, when
her mammo-
gram revealed
calcifications in
the left breast.
The radiologist
wanted more
images, then
an ultrasound.
Cindy realized that the radiologist had seen something sus-
picious and, waiting for the technician in the ultrasound
room, she was alone with her thoughts. The images were
enough to require a biopsy at the Medical University of
South Carolina.
“They try to let you know within 48 hours,” Cindy said.
Luckily, she had a friend who told her within 24 hours
that it was indeed breast cancer. The mother of a young
son, Cindy began to worry about the future. She had a
double mastectomy Aug. 29. She did not require chemo-
therapy but found that medication would be a part of her
life for 10 years.
“I was on Tamoxifen but I had side effects,” she said. “I
was not feeling well.”
Cindy is on Letrazole, a drug that is used for hormone-
receptor-positive breast cancers, but said this drug, too, has
side effects.
“I have joint pain, brain fog and cognitive issues,” she said.
In spite of the emotional rollercoaster of the treatment,
Cindy is grateful.
“It was stage 1 and it was caught early,” she said.
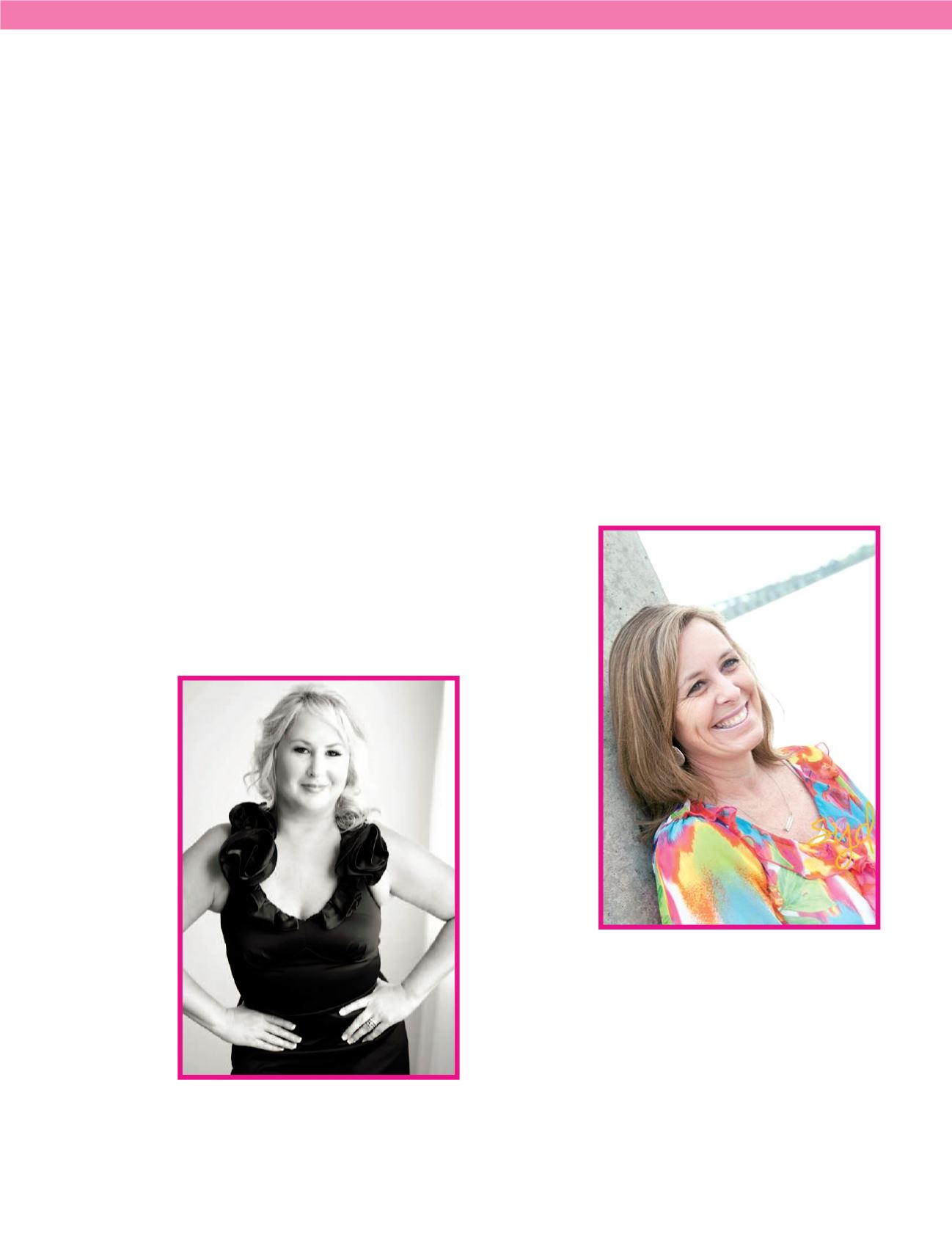
life maTTerS
“On April 9,
2015, I had an
appointment for
a mammogram,”
Cara Fowler
said. “That
morning I felt
a lump in the
shower.”
It seemed
just as well.
Cara figured
she’d have that
checked out
during her ap-
pointment, but
she was told that
would require
a different ap-
pointment and
one was made for the next morning.
“I turned to go, then stopped and asked ‘Do I need my
husband with me?’”
The answer was yes. Her husband, meteorologist Rob
Fowler, changed his plans to accompany her.
The next morning she learned that there was probable
cancer. And so began the whirlwind. She had two biopsies,
which confirmed the cancer diagnosis: triple negative inva-
sive ductal carcinoma.
She decided to consult her friend and neighbor, Dr.
Megan Baker, who was then a breast surgeon at the Medical
University of South Carolina (She is now a Roper St. Francis